Use of Augmented Reality as a Radiation-free Alternative in Pain Management Spinal Surgeries
Introduction
The field of Anesthesiology has consistently evolved, incorporating advanced technologies to improve patient care and surgical outcomes. One of the most groundbreaking advancements in recent years is the application of Augmented Reality (AR) in spinal surgeries. The study titled “Use of Augmented Reality as a Radiation-free Alternative in Pain Management Spinal Surgeries” highlights the transformative potential of AR systems as cost-effective and radiation-free tools. This blog delves into the study’s findings and explores their implications for anesthesiology and beyond.
Why Augmented Reality in Spinal Surgeries?
Traditional spinal surgeries heavily rely on fluoroscopy for imaging guidance. However, prolonged exposure to radiation poses risks for both patients and surgical teams. The integration of AR technology offers a safer, cost-effective alternative. With the ability to overlay virtual 3D anatomical models onto physical patients, AR eliminates the need for fluoroscopy, significantly reducing radiation exposure.
Key Benefits of AR in Spinal Surgeries:
- Radiation-free procedures: Ensures a safer surgical environment.
- Cost-effectiveness: AR systems cost a fraction of traditional navigation setups.
- Enhanced precision: Real-time visualization aids in accurate needle placement.
The implications of these advancements are profound, particularly in Anesthesiology, where precision and safety are paramount.
Methodology: How AR Revolutionizes Spinal Surgery
Simplified Spinal Model
The study utilized a simplified spinal model, comprising a 3D-printed cylinder encased in ballistic gel, to simulate the human spine and body. A metal detector embedded within the model provided real-time feedback, indicating successful needle placement.
AR Setup
A commercially available AR headset (Meta Quest 3) was employed, offering affordability and accessibility. Using MRI imaging and CAD modeling, a virtual spine was created and overlaid onto the physical model. This approach allowed surgeons to navigate the anatomy with unparalleled accuracy, without relying on radiation-based imaging tools.
Experimental Results
The study’s findings demonstrated the efficacy of AR in improving surgical precision:
- Success Rate: AR guidance increased the success rate of needle placement by 40% compared to non-AR methods.
- Accuracy: The average deviation from the target decreased by 50% with AR assistance.
These results underscore AR’s potential to revolutionize Anesthesiology practices by enhancing procedural accuracy and safety.
Implications for Anesthesiology
In the realm of Anesthesiology, AR technology offers significant advantages, particularly in pain management procedures. Spinal injections, a common intervention for managing chronic pain, require precise needle placement to avoid complications and maximize efficacy. AR-guided systems provide anesthesiologists with:
- Real-time visualization: Enables accurate navigation of complex spinal anatomy.
- Minimized risks: Reduces the likelihood of nerve damage or misplacement.
- Improved outcomes: Enhances patient satisfaction and procedural success rates.
Moreover, the affordability of AR systems ensures that these benefits can be extended to smaller healthcare facilities, democratizing access to advanced surgical tools.
Challenges and Future Directions
While the potential of AR in Anesthesiology is undeniable, several challenges remain:
- Integration with Existing Systems: Seamlessly incorporating AR with other surgical tools and workflows requires further refinement.
- Real-world Variables: Factors such as patient movement, anatomical variations, and environmental conditions must be addressed to enhance AR accuracy.
- Training and Adoption: Ensuring that anesthesiologists and surgeons are adequately trained to use AR systems is critical for widespread adoption.
Future Developments
The study suggests several avenues for future research and development:
- Convolutional Neural Networks (CNNs): Leveraging AI to reconstruct MRI models with greater accuracy.
- Advanced Instrumentation: Integrating trackable surgical instruments for real-time monitoring.
- Enhanced Modeling: Developing more realistic anatomical models to improve system robustness.
Broader Applications of AR in Medicine
Beyond spinal surgeries, AR technology holds promise for various applications within Anesthesiology and other medical fields:
Education and Training
AR can serve as a powerful educational tool, allowing anesthesiology trainees to practice complex procedures in a risk-free environment. By overlaying virtual models onto physical mannequins, AR provides hands-on learning opportunities that closely mimic real-world scenarios.
Pain Management
In chronic pain management, AR-guided interventions can improve the precision of nerve blocks and epidural injections, enhancing patient outcomes while minimizing risks.
Surgical Planning
For complex surgeries, AR enables detailed preoperative planning by visualizing patient-specific anatomy. This capability is particularly beneficial in cases involving anatomical anomalies or previous surgical interventions.
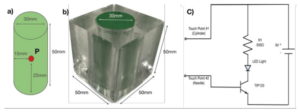 Figure: Simplified spinal model with a detection feedback circuit. a) Cylinder representing the spine. b) Cylinder encased in gel representing the body of the patient. c) Circuit for detecting contact.
Figure: Simplified spinal model with a detection feedback circuit. a) Cylinder representing the spine. b) Cylinder encased in gel representing the body of the patient. c) Circuit for detecting contact.
Conclusion
The integration of Augmented Reality into Anesthesiology represents a paradigm shift, offering safer, more precise, and cost-effective solutions for spinal surgeries and beyond. The findings of the referenced study highlight the transformative potential of AR systems, paving the way for widespread adoption in medical practice.
As the technology continues to evolve, the keywords “Anesthesiology” and “innovation” will remain at the forefront of discussions, symbolizing the relentless pursuit of excellence in patient care. By embracing AR, the medical community can redefine what is possible in surgical precision and patient safety.
