Investigating the Causal Link Between Lipid-Lowering Medications and Malignant Meningiomas Using Drug-Target Mendelian Randomization Analysis
Introduction
Malignant meningiomas are rare but aggressive brain tumors that pose significant challenges in treatment and prognosis. Classified as Grade II or III by the World Health Organization (WHO), these tumors often recur after treatment, necessitating innovative approaches to prevention and management. Current treatment options, such as surgery and radiotherapy, have limitations, driving the need for alternative strategies.
Recent advancements in genetic epidemiology, particularly Mendelian Randomization (MR), have enabled researchers to explore causal relationships between various exposures and diseases. Among these, the relationship between lipid-lowering medications and tumor risk has garnered attention. Statins, commonly prescribed for cardiovascular diseases, are hypothesized to have a protective role against certain cancers, including malignant meningiomas. This blog delves into a groundbreaking study that utilizes MR to investigate this potential link and its implications for oncology.
Understanding Mendelian Randomization
Mendelian Randomization (MR) is a method that uses genetic variants as proxies (instrumental variables) to explore causal relationships between risk factors and health outcomes. Unlike traditional observational studies, MR minimizes bias by leveraging the random allocation of genes at conception, reducing confounding and reverse causation.
In this study, MR was applied to assess whether genetic variations associated with lipid-lowering drug targets—HMG-CoA reductase (HMGCR), PCSK9, NPC1L1, and APOB—are linked to the risk of malignant meningiomas. These genetic proxies represent the biological effects of statins and other lipid-lowering therapies, providing valuable insights into their potential role in cancer prevention.
Study Objectives and Methods
The primary objective of the study was to determine whether lipid-lowering drugs, particularly statins targeting HMGCR, reduce the risk of malignant meningiomas. The research employed genetic and epidemiological data from large-scale Genome-Wide Association Studies (GWAS) and the FinnGen biobank.
Key Components of the Methodology:
- Selection of Genetic Instruments: Genetic variants near HMGCR, PCSK9, NPC1L1, and APOB genes were used as proxies for the effects of lipid-lowering drugs.
- Data Sources: GWAS data on malignant meningiomas and lipid-related traits were obtained from publicly available datasets, ensuring robust sample sizes.
- Statistical Analyses: Multiple MR methods, including Inverse Variance Weighting (IVW), were used to estimate the association between genetic proxies and tumor risk. Sensitivity analyses ensured the robustness of findings.
Key Findings
HMGCR as a Protective Factor:
- Genetic variants associated with increased HMGCR expression were linked to a lower risk of malignant meningiomas.
- The IVW analysis demonstrated a significant association, with statin use reducing the odds of developing these tumors (Odds Ratio = 2.57, p = 0.039).
Other Lipid-Lowering Targets:
- No significant associations were observed for PCSK9, NPC1L1, or APOB, suggesting that the protective effect is specific to HMGCR inhibition.
Validation and Robustness:
- Sensitivity analyses confirmed the reliability of the findings, with minimal evidence of bias or pleiotropy.
These results strongly support the hypothesis that statins, through their inhibition of HMGCR, may play a role in preventing malignant meningiomas.
Mechanisms Underlying the Protective Role of Statins
Statins primarily function by inhibiting HMGCR, the rate-limiting enzyme in cholesterol biosynthesis. Beyond their lipid-lowering effects, statins exhibit anti-inflammatory and anti-proliferative properties that may contribute to their protective role in cancer:
- Cholesterol Deprivation: Cancer cells rely on cholesterol for membrane synthesis and energy production. Statins disrupt this pathway, potentially hindering tumor growth.
- Anti-Inflammatory Effects: Chronic inflammation is a known risk factor for cancer. Statins reduce systemic inflammation, lowering the tumor-promoting environment.
- Inhibition of Angiogenesis: Statins impede the formation of new blood vessels, a critical process for tumor growth and metastasis.
These pleiotropic effects make statins promising candidates for repurposing in oncology.
Implications for Clinical Practice
Drug Repurposing:
Statins are widely used, well-studied, and cost-effective. Their potential role in cancer prevention represents an opportunity to repurpose an existing drug for a new therapeutic indication.Personalized Medicine:
Genetic insights from MR can guide personalized treatment strategies, identifying individuals who may benefit most from statin therapy.Integration with Current Therapies:
Statins could complement existing treatments for malignant meningiomas, enhancing efficacy while reducing recurrence rates.
Challenges and Limitations
Despite its strengths, the study faced several challenges:
- Population-Specific Findings: The analysis was based on data from European populations, limiting generalizability to other ethnic groups.
- Statistical Power: While significant, the confidence intervals for some estimates were wide, highlighting the need for larger datasets.
- Mechanistic Understanding: The precise biological mechanisms linking statin use to tumor suppression remain unclear, necessitating further research.
Future Directions
The findings of this study open new avenues for research and clinical exploration:
Clinical Trials:
Randomized controlled trials are essential to validate the protective effects of statins against malignant meningiomas and determine optimal dosing strategies.Mechanistic Studies:
Investigating the molecular pathways involved in HMGCR inhibition and tumor suppression will enhance our understanding and identify potential targets for new therapies.Expanding MR Applications:
The use of MR can be extended to explore the effects of other drugs and genetic factors on cancer risk, broadening the scope of drug repurposing.
Case for Statin Use in Oncology
The results of this study align with a growing body of evidence suggesting the anti-cancer properties of statins. While their primary role remains in cardiovascular disease management, the potential to reduce the risk of malignant meningiomas and other cancers represents a significant breakthrough in oncology.
Given their affordability, safety profile, and widespread availability, statins could become a cornerstone of cancer prevention strategies, particularly for high-risk populations.
Conclusion
This study demonstrates the potential of statins to reduce the risk of malignant meningiomas through Mendelian Randomization analysis. By leveraging genetic data, it establishes a causal link between HMGCR inhibition and tumor risk reduction, paving the way for innovative approaches to cancer prevention.
While further research is needed to confirm these findings and explore their clinical implications, the study represents a significant step forward in understanding the intersection of lipid metabolism and cancer. The integration of genetic epidemiology with therapeutic development holds immense promise for addressing some of the most pressing challenges in modern medicine.
Tags:
#Statins #MalignantMeningiomas #MendelianRandomization #CancerPrevention #LipidMetabolism #DrugRepurposing #Oncology #GeneticEpidemiology #CholesterolAndCancer #PublicHealthInnovation
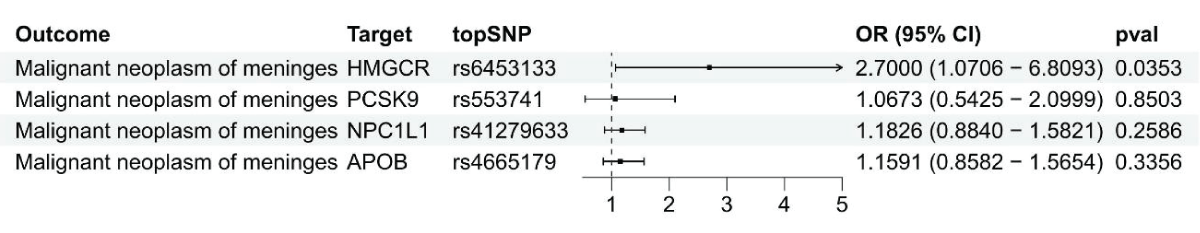
Using summary data, a Mendelian Randomization analysis was conducted to investigate the link between gene expression levels of HMGCR, PCSK9, NPC1L1, and APOB and malignant meningiomas.
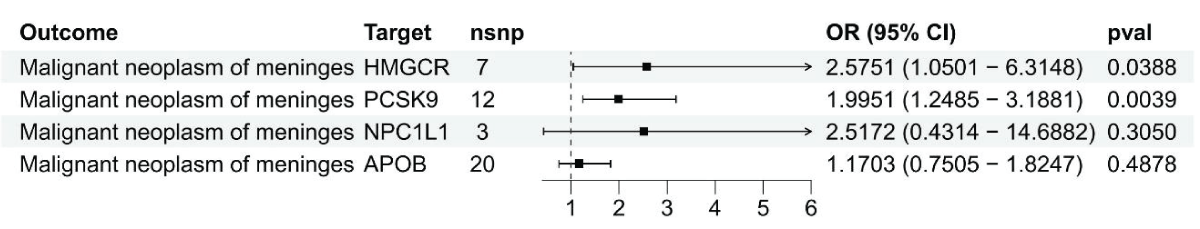
Results from the Inverse-Variance Weighted (IVW) method in Figure 2 show the connection between LDL cholesterol and malignant meningiomas through HMGCR, PCSK9, NPC1L1, and APOB genes.
