Country Risk in Global Emergencies: The Adverse Impact of High Public Debt on Health Expenditures and Mortality Rates During the COVID-19 Pandemic
Introduction
The COVID-19 pandemic has highlighted numerous vulnerabilities in global public health systems, with countries across the world struggling to respond to the healthcare demands of the crisis. One of the critical factors that have influenced the ability of nations to manage public health during the pandemic is the level of public debt. Countries with higher levels of public debt have faced greater challenges in managing the economic burden of the pandemic, particularly with respect to public health expenditures and the ability to reduce COVID-19 fatality rates. The relationship between public debt and public health expenditures is an area that requires in-depth exploration, especially as the world prepares for future global health emergencies.
In this blog post, we will delve into the findings of a study that explores the negative effects of high public debt on public health systems, with a focus on European countries and the devastating impact of COVID-19. The study assesses how high public debt reduces health spending, making countries more vulnerable to global health crises. Furthermore, the post will provide insight into the implications of this relationship for future public health preparedness and crisis management.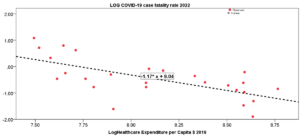
Figure 1: Regression line of the COVID-19 fatality rate in 2022 on healthcare expenditures per capita in 2019.
Public Debt and Public Health: An Inextricable Link
Public debt refers to the total amount of money that a government owes, often incurred through borrowing to fund projects or manage deficits. While public debt can be necessary for a country’s economic growth, excessive debt can have long-term consequences, especially when it comes to public health. High levels of public debt often lead to austerity measures, including cuts in essential public services like healthcare, education, and social welfare. In times of crisis, such as the COVID-19 pandemic, countries burdened by high debt often find it challenging to allocate sufficient resources to public health initiatives, which can have dire consequences on the health of the population.
During the COVID-19 pandemic, the study highlighted in this post reveals that countries with higher levels of public debt saw a greater fatality rate from the virus. This correlation is attributed to the reduced ability of these nations to invest adequately in healthcare systems due to their fiscal constraints. When public health expenditures are reduced, healthcare systems are less prepared to handle a health crisis of this magnitude, leading to higher mortality rates. The study also emphasizes the negative feedback loop: countries with higher debt struggle to increase healthcare spending, which, in turn, increases vulnerability during future health crises.
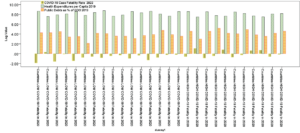
Figure 2: Comparison of COVID-19 fatality rate in 2022, health expenditure per capita in 2019 and level of public debt in European countries of group 1 (Countries with LOWER COVID-19 Fatality in 2020) and group 2 (Countries with HIGHER COVID-19 Fatality in 2020).
European Case Study: High Public Debt and Health Outcomes
The study focused on a group of 27 European countries, all with similar socioeconomic systems, to analyze the effects of public debt on health expenditures and COVID-19 fatality rates. These countries were categorized into two groups based on their COVID-19 fatality rates in 2020. The first group consisted of countries with lower fatality rates, while the second group consisted of countries with higher fatality rates.
Group 1: Countries with lower COVID-19 fatality rates had higher public health expenditures per capita, with an average expenditure greater than $3,100 per person. These countries also experienced a lower rate of public debt growth, which helped them maintain strong healthcare systems during the pandemic. The study found that these nations were better equipped to manage the health crisis, resulting in a lower mortality rate.
Group 2: Countries with higher COVID-19 fatality rates had lower health expenditures per capita (around $2,500 per person). These countries also experienced a higher rate of public debt growth, which led to cuts in public health funding. As a result, their healthcare systems were less prepared for the pandemic, contributing to higher fatality rates.
The findings from this analysis underscore the direct relationship between public health expenditures, public debt, and COVID-19 outcomes. Countries with lower public debt and higher healthcare spending were better positioned to face the challenges posed by the pandemic, proving that investment in public health infrastructure is a critical factor in mitigating the impact of global emergencies.
The Role of Public Health Expenditures in Crisis Response
Public health expenditures play a crucial role in a country’s ability to respond to global emergencies, such as the COVID-19 pandemic. These expenditures support healthcare infrastructure, including hospital beds, medical equipment, and emergency response services. During the COVID-19 pandemic, nations with higher public health investments were able to allocate more resources to testing, vaccination campaigns, and the treatment of critically ill patients.
The study reveals that for every 1% increase in healthcare expenditure per capita, countries experienced a 1.2% reduction in COVID-19 fatality rates. This statistical finding further emphasizes the importance of sustained investment in public health as a means of reducing mortality and improving outcomes during health crises.
The regression analysis conducted in the study supports this relationship, showing that healthcare expenditure per capita is a reliable predictor of COVID-19 fatality rates. This suggests that countries that have historically invested in robust public health systems are more resilient during global health emergencies. It also implies that public health policy needs to prioritize long-term investments in healthcare infrastructure, especially in times of economic uncertainty and rising public debt.
Public Debt and Vulnerability to Future Emergencies
The implications of high public debt on public health are not limited to the COVID-19 pandemic. Countries with high levels of public debt are more likely to struggle with funding healthcare systems during future global emergencies, whether they be pandemics, natural disasters, or conflicts. The study suggests that reducing public debt and improving fiscal governance are critical steps in enhancing a country’s ability to cope with unforeseen crises.
In particular, health systems resilience is a key factor in determining how well a country can respond to global health threats. High public debt can lead to weakened health systems, with fewer resources available to invest in emergency preparedness, pandemic control measures, and health interventions. The result is heightened vulnerability, not only to COVID-19 but also to future infectious disease outbreaks.
The European Central Bank and other international bodies have stressed the importance of reducing public debt through sound fiscal policies while maintaining adequate funding for public health. This balance is essential for ensuring that nations are better prepared to face the next global emergency.
Policy Recommendations: Strengthening Public Health Systems
Based on the findings of this study, several key policy recommendations are suggested to strengthen public health systems and reduce the impact of public debt on health outcomes:
Invest in Health Infrastructure: Governments should prioritize investments in public health systems, especially during times of economic stability. This will ensure that health systems are resilient enough to handle future crises.
Reduce Public Debt: Countries should implement policies that aim to reduce public debt over the long term, allowing for more flexibility in healthcare spending during emergencies.
Focus on Preventive Health: Preventive health measures, such as vaccination programs and public health education, should be a core focus of public health policy to reduce the burden on healthcare systems during pandemics.
Improve International Cooperation: Global health crises like the COVID-19 pandemic require international cooperation. Countries must work together to share resources, information, and support, particularly in regions with lower public health resources.
Adopt Sustainable Financial Strategies: Governments should move away from austerity measures that cut healthcare spending and adopt more sustainable financial strategies that allow for adequate investment in public health.
Conclusion
The COVID-19 pandemic has exposed the critical role that public health expenditures play in mitigating the effects of global health crises. Countries with lower public debt and higher healthcare spending were more resilient in the face of the pandemic, while those with high public debt struggled to provide the necessary resources to control the virus and save lives.
As we look ahead to future global emergencies, it is clear that public health must be prioritized. Investments in healthcare systems, reduction in public debt, and the implementation of proactive public health policies will ensure that countries are better prepared to face whatever challenges lie ahead. Ultimately, the lessons learned from the COVID-19 pandemic must inform future public health strategies to build more resilient, sustainable, and effective health systems worldwide.
FAQ’s:
How does public debt affect public health during crises?
A: High public debt limits healthcare spending, making it harder to manage health crises like the COVID-19 pandemic.What is the relationship between public health spending and fatality rates?
A: Higher public health expenditures are linked to lower fatality rates, as better-funded healthcare systems can respond more effectively.How does public debt influence future health emergencies?
A: High public debt reduces a country’s ability to invest in health infrastructure, leaving it vulnerable in future health emergencies.What are the benefits of reducing public debt for public health?
A:Reducing public debt allows for increased healthcare funding, enhancing health system resilience during global emergencies.What policies can improve public health preparedness?
A: Policies should focus on health infrastructure investment, debt reduction, and international cooperation for better health crisis management.
