EB Naevi-Like Lesions in Infantile Bullous Pemphigoid
A Comprehensive Study of EB Naevi-Like Lesions in Infant Bullous Pemphigoid: Insights from Dermatology, Pediatrics, and Internal Medicine
The intersection of dermatology, pediatrics, and internal medicine creates a rich landscape for diagnosing and managing rare and complex conditions. One such condition is Infant Bullous Pemphigoid (BP), a rare autoimmune disease characterized by subepidermal blistering. In an even rarer subset of cases, BP may lead to the development of EB Naevi (EBN)-like lesions, which pose unique diagnostic and therapeutic challenges.
This blog post examines a recent case study published in the “EB Naevi-Like Lesion in Infant Bullous Pemphigoid” research article. It explores the clinical, diagnostic, and therapeutic considerations necessary for managing this rare presentation, while emphasizing how dermatology, pediatrics, and internal medicine collaboratively address such complex cases.
Introduction to Bullous Pemphigoid and Epidermolysis Bullosa Naevi
Bullous Pemphigoid: A Rare Dermatological and Pediatric Concern
Bullous Pemphigoid (BP) is an autoimmune blistering disease primarily affecting the elderly, with only rare cases documented in pediatric populations. In infants, BP often presents with:
- Large, tense blisters containing serous or hemorrhagic fluid.
- Erythematous plaques with intense pruritus.
- A better therapeutic response compared to adult cases, but still challenging to diagnose due to its rarity.
The diagnosis and management of BP require expertise in dermatology to evaluate skin lesions, pediatrics to account for age-specific factors, and internal medicine to manage systemic involvement.
Epidermolysis Bullosa Naevi
EBN refers to pigmented lesions that arise in areas of recurrent blistering. Originally described in patients with Epidermolysis Bullosa (EB), these lesions mimic melanoma in their clinical and dermoscopic features. Key characteristics include:
- Irregular pigmentation.
- Satellite lesions.
- A benign clinical course despite initial alarming features.
EBN and EBN-like lesions have been reported in other conditions, including Stevens-Johnson Syndrome, erythema multiforme, and, as in this case, Bullous Pemphigoid.
 Figure 1: Urticarial plaques, some arciforms; tense bullous lesions in trunk, limbs, and face; exulcerations and hematic crusts.
Figure 1: Urticarial plaques, some arciforms; tense bullous lesions in trunk, limbs, and face; exulcerations and hematic crusts.
Case Highlights: A Collaboration Between Dermatology, Pediatrics, and Internal Medicine
The case involves a 5-month-old boy presenting with classic BP symptoms and later developing EBN-like lesions. It illustrates how the expertise of dermatology, pediatrics, and internal medicine converges to provide comprehensive care.
Figure 2: Pigmented macule, with heterogeneous brownish coloration, irregular contour, and satellite-dotted lesions, located on the right flank.
Clinical Presentation
The child presented with:
- Erythematous macules and tense blisters initially on the lower limbs and trunk, spreading to the face, hands, and feet.
- Urticarial plaques with crusting but no systemic symptoms.
- A history of recent vaccination with the pneumococcal conjugate and inactivated poliovirus vaccines, a potential trigger for BP.
Diagnostic Approach
The diagnosis of BP was established through:
- Histopathology (Dermatology):
- Subepidermal blisters with eosinophilic infiltrates.
- Direct Immunofluorescence (Dermatology):
- Linear deposits of IgG and C3 along the basement membrane.
- Pediatric Assessment:
- A thorough evaluation to rule out other blistering conditions common in infants.
- Internal Medicine Support:
- Ensuring systemic stability and ruling out broader autoimmune implications.
The Emergence of EBN-Like Lesions
After the resolution of bullous lesions, a pigmented lesion resembling EBN developed on the child’s flank. This lesion was characterized by:
- Irregular borders, heterogeneous pigmentation, and satellite spots.
- A reticular dermoscopic pattern interspersed with healthy skin.
Management Decision
Instead of invasive surgical intervention, a conservative approach of observation and follow-up was chosen. The lesion regressed over 24 months, highlighting the importance of cautious decision-making in pediatric dermatology and internal medicine.
Pathophysiology: Bridging Dermatology and Internal Medicine
The pathogenesis of EBN-like lesions in BP involves complex mechanisms that bring together insights from dermatology and internal medicine:
- Repeated Trauma Hypothesis:
- Chronic blistering damages the basal epidermal layer, triggering melanocyte proliferation during healing.
- Inflammatory Environment:
- Cytokines and growth factors, such as hepatocyte growth factor (HGF), found in blister fluid promote pigmentation.
This understanding underscores the interplay between immune dysregulation and skin pathology, central to both dermatology and internal medicine.
Diagnostic Challenges and Strategies
Challenges in Diagnosis
EBN-like lesions mimic melanoma in several ways:
- Irregular pigmentation and asymmetry.
- Satellite stippling, which raises concerns about malignancy.
The Role of Dermatology in Diagnosis
Dermoscopy is an invaluable tool in distinguishing benign from malignant lesions. Dermatologists rely on:
- Reticular patterns and pigmentation distribution to identify EBN.
- Longitudinal monitoring to confirm benign progression.
The Contribution of Pediatrics and Internal Medicine
Pediatricians ensure that developmental and immunization histories are considered in the diagnostic process. Internal medicine specialists monitor for systemic manifestations that might complicate or misdirect the diagnosis.
Management Principles: Collaboration Across Specialties
Dermatology’s Role
- Providing targeted treatments for skin lesions, such as topical steroids or immunomodulators.
- Leveraging advanced diagnostic tools like dermoscopy and biopsy when necessary.
Pediatric Contributions
- Ensuring age-appropriate dosing and monitoring of systemic medications.
- Counseling families on the benign nature of EBN-like lesions to alleviate concerns.
Internal Medicine’s Perspective
- Addressing systemic complications such as infections or inflammation.
- Supporting interdisciplinary management of autoimmune components.
Treatment Pathway
Initial Management
- Prednisolone (1 mg/kg/day) for inflammation control.
- Cephalexin and hydroxyzine for infection prevention and symptom relief.
Escalation in Care
Due to worsening lesions, the following steps were taken:
- Addition of Dapsone:
- An immunomodulator commonly used in dermatological conditions.
- Hospitalization:
- Intravenous antibiotics (vancomycin, cefepime) and immunoglobulin therapy.
- Corticosteroid adjustments, transitioning to betamethasone for improved outcomes.
Implications for Clinical Practice
For Dermatologists
Understanding EBN-like lesions in bullous conditions prevents unnecessary invasive procedures. Dermatologists play a pivotal role in ensuring accurate diagnosis and monitoring.
For Pediatricians
Pediatricians must consider BP and EBN in differential diagnoses for blistering and pigmented lesions. Their involvement ensures that treatments are safe and effective for young patients.
For Internal Medicine Specialists
The systemic nature of autoimmune disorders like BP often requires internal medicine oversight to manage potential complications and coexisting conditions.
Guidelines for Long-Term Monitoring
Regular Follow-Up:
- Monitor lesions for signs of regression or unexpected changes.
- Ensure ongoing collaboration between dermatology, pediatrics, and internal medicine.
Family Education:
- Counsel families on the benign nature of EBN-like lesions to reduce anxiety and promote adherence to follow-up schedules.
Data Collection:
- Document cases to contribute to the limited body of literature on pediatric BP and EBN-like lesions.
Future Directions
Research Opportunities
The case highlights several areas for future investigation:
- Long-term outcomes of EBN-like lesions in bullous conditions.
- Molecular studies on cytokines and growth factors driving lesion formation.
Advancing Diagnostics
Innovations in imaging and molecular diagnostics could improve the differentiation between benign and malignant pigmented lesions, benefitting dermatology and internal medicine practices.
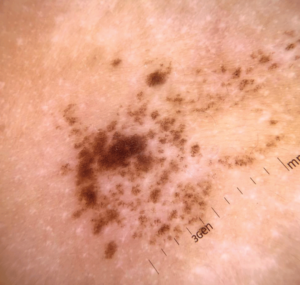
Figure 3 : Dermoscopy: a reticular lesion with a regular pigmented network distributed in an agminated manner, interspersed with areas of healthy skin.Developing Pediatric-Specific Guidelines
Establishing standardized protocols for pediatric BP will enhance care and streamline interdisciplinary management.
Conclusion
The case of EB Naevi-like lesions in infant Bullous Pemphigoid showcases the vital collaboration between dermatology, pediatrics, and internal medicine. By understanding the clinical and systemic intricacies of this condition, healthcare providers can deliver accurate diagnoses and effective treatments while avoiding unnecessary interventions. As research continues to expand, the hope is to refine diagnostic and management strategies further, improving outcomes for young patients with rare and complex conditions.
Tags
- Pediatric Dermatology
- Autoimmune Skin Disorders
- Epidermolysis Bullosa Naevi
- Internal Medicine and Skin Diseases
- Rare Pediatric Conditions
- Skin Lesion Diagnosis
- Interdisciplinary Patient Care
- Bullous Pemphigoid in Infants
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
