Mastocytosis: Principles and Pitfalls in the Diagnosis of a Unique Disease
Haematology and Pathology – Principles and Pitfalls in Diagnosing Mastocytosis
Haematology and Pathology are integral fields in understanding and diagnosing rare and complex diseases. Mastocytosis, a unique hematological neoplasm characterized by abnormal mast cell proliferation, poses diagnostic challenges due to its diverse clinical and histomorphological manifestations. This blog explores the principles, pitfalls, and advancements in diagnosing systemic mastocytosis (SM), as discussed in a recent comprehensive review.
For more details, refer to the HTML article or the PDF version.
Introduction
Mastocytosis comprises a range of disorders caused by the clonal proliferation of mast cells, which accumulate in the skin (cutaneous mastocytosis) or extracutaneous organs (systemic mastocytosis). It is listed as a distinct entity in the 5th edition of the WHO classification and the 2022 International Consensus Classification. This blog focuses on systemic mastocytosis (SM), its subtypes, and the evolving diagnostic methodologies in Haematology and Pathology.
Key Features of Mastocytosis
1. Types of Mastocytosis
- Cutaneous Mastocytosis (CM): Confined to the skin, primarily affects children, and has a favorable prognosis.
- Systemic Mastocytosis (SM): Involves extracutaneous organs and is classified into non-advanced (e.g., indolent SM) and advanced (e.g., aggressive SM, mast cell leukemia) forms.
2. Clinical Challenges
- Symptoms range from skin lesions and anaphylaxis to severe organ dysfunction, making early and accurate diagnosis critical.
Diagnostic Principles in Haematology and Pathology
1. Updated Diagnostic Criteria
The diagnosis of SM is based on the 2022 WHO and ICC criteria:
- Major Criterion: Multifocal dense infiltrates of mast cells (≥15 cells per aggregate) in bone marrow or other organs.
- Minor Criteria:
- KIT mutations (e.g., D816V).
- Spindle-shaped or atypical mast cells in ≥25% of infiltrates.
- Aberrant antigen expression (e.g., CD25, CD30).
- Elevated serum tryptase (>20 ng/mL).
A diagnosis requires at least one major and one minor criterion or three minor criteria.
2. Histomorphology and Immunohistochemistry
Histomorphological analysis of bone marrow is essential, supported by stains like Giemsa and toluidine blue to detect mast cell granules. Immunohistochemical markers such as CD117 (KIT) and tryptase are critical for identifying atypical mast cells.
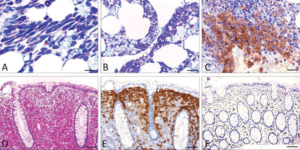
Figure 1: Basic features of SM (A-C; bone marrow infiltrate and D-F; infiltrate of the colon).
Pitfalls in Diagnosis
- Overlapping Features
- Mast cell infiltrates may mimic lymphomas or other hematological disorders, leading to misdiagnosis.
- Aberrant antigen expression can blur diagnostic boundaries.
- KIT Mutation Challenges
- KIT mutations like D816V are found in 90% of SM cases but may require sensitive methods (e.g., digital-droplet PCR) for detection.
- Variability in Presentation
- Subtypes like indolent SM may have minimal symptoms, while aggressive SM can cause severe organ dysfunction.
Advancements in Haematology and Pathology
- Tyrosine Kinase Inhibitors (TKIs)
- Targeting KIT mutations, TKIs like midostaurin have revolutionized SM treatment, particularly for advanced cases.
- Molecular Techniques
- Advanced genetic testing for KIT and secondary mutations (e.g., ASXL1, SRSF2) aids in risk stratification and treatment planning.
- Multidisciplinary Approaches
- Collaboration between hematopathologists, haemato-oncologists, and molecular biologists ensures accurate diagnosis and effective management.
Subtypes of Systemic Mastocytosis
- Indolent SM (ISM):
- Most common subtype, affecting 80% of SM patients.
- Typically involves the skin and bone marrow with minimal organ dysfunction.
- Aggressive SM (ASM):
- Characterized by extensive organ involvement and significant morbidity.
- Mast Cell Leukemia (MCL):
- The rarest and most severe subtype, diagnosed by cytomorphology alone when mast cells exceed 20% of nucleated cells in bone marrow.

Figure 2: Diagnostic workup of a patient with suspected mastocytosis
- The rarest and most severe subtype, diagnosed by cytomorphology alone when mast cells exceed 20% of nucleated cells in bone marrow.
Implications for Haematology and Pathology
- Improving Diagnostic Accuracy
- Standardized criteria and advanced techniques reduce misdiagnosis and improve patient outcomes.
- Enhanced Treatment Strategies
- Precision medicine approaches, including targeted therapies, are transforming the management of SM.
- Future Research Directions
- Developing more sensitive diagnostic tools and exploring the role of novel mutations in SM pathogenesis.
Conclusion
The diagnosis of mastocytosis requires expertise in Haematology and Pathology, supported by advanced molecular and histopathological techniques. Accurate diagnosis not only improves patient care but also facilitates the use of emerging therapies, such as TKIs. This comprehensive approach underscores the importance of multidisciplinary collaboration in tackling this rare and complex disease.
For a deeper understanding, visit the HTML article or access the PDF version.
