Peritoneal Carcinomatosis from Ovarian Cancer: A Case Report
Advances in Managing Peritoneal Carcinomatosis from Ovarian Cancer
Epithelial ovarian cancer remains the leading cause of death from gynecologic malignancies in Western countries. With a high rate of late-stage diagnosis and locoregional spread to the peritoneum, survival rates are dismal without aggressive treatment. However, recent advances in multimodal therapies, including cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC), offer new hope for patients. This blog explores a detailed case report and highlights the cutting-edge strategies for managing peritoneal carcinomatosis from ovarian cancer, as discussed in “Peritoneal Carcinomatosis from Ovarian Cancer” and its associated DOI reference.
Understanding Peritoneal Carcinomatosis
Peritoneal carcinomatosis occurs when cancer cells spread across the peritoneal surface, commonly observed in advanced ovarian cancer. Patients often present with symptoms like abdominal pain, distention, nausea, and weight loss, as in the featured case of a 49-year-old woman diagnosed with Stage IIIC endometrioid carcinoma.
Case Summary: A Patient’s Journey
The case report details a 49-year-old woman presenting with abdominal pain, distention, and constitutional symptoms. Imaging revealed large vascularized ovarian masses, with ascitic fluid indicating peritoneal carcinomatosis. The patient underwent:
- Bilateral Adnexectomy: Removal of both ovaries and associated tissues, revealing moderately differentiated endometrioid carcinoma.
- Neoadjuvant Chemotherapy: A regimen of Carboplatin and Paclitaxel, leading to significant radiologic improvement.
- Interval Cytoreductive Surgery and HIPEC: Surgery combined with intraperitoneal cisplatin-based chemotherapy at 42°C to maximize tumor clearance and reduce recurrence.
Postoperative outcomes were favorable, with no recurrence observed in follow-up imaging two months after surgery.
The Role of Cytoreductive Surgery and HIPEC
Cytoreductive Surgery
This aggressive surgical approach aims to remove visible tumors from the peritoneal cavity. Procedures often include peritonectomy, omentectomy, and hysterectomy, tailored to achieve maximal tumor reduction.
HIPEC: Hyperthermic Intraperitoneal Chemotherapy
HIPEC is administered during surgery to eliminate residual microscopic disease. Benefits include:
- Enhanced Drug Penetration: Hyperthermia improves the efficacy and penetration of chemotherapy agents.
- Reduced Systemic Toxicity: The peritoneal-plasma barrier localizes drug activity, minimizing side effects.
Clinical trials, including the Dutch study (NCT00426257), have shown that HIPEC after interval cytoreductive surgery significantly improves recurrence-free and overall survival in Stage III ovarian cancer.
Clinical Evidence Supporting HIPEC
Several studies underscore the transformative potential of HIPEC in ovarian cancer treatment:
- Dutch Trial (NCT00426257):
- Included 245 patients with Stage III ovarian cancer.
- HIPEC added to interval surgery extended overall survival to 45.7 months compared to 33.9 months with surgery alone.
- ESMO-ESGO Meta-Analysis (2022):
- HIPEC after neoadjuvant chemotherapy significantly increased 5-year survival rates in advanced ovarian cancer.
- NCCN Guidelines:
- HIPEC is now a recommended option for Stage III patients responding to neoadjuvant chemotherapy, marking a pivotal shift in ovarian cancer management.
Challenges and Future Directions
While HIPEC represents a promising treatment modality, challenges remain:
- Resource-Intensive: Requires specialized surgical expertise and equipment.
- Patient Selection: Identifying candidates who will benefit most from HIPEC is crucial.
- Recurrence Risk: Microscopic disease still poses a recurrence risk, necessitating ongoing innovation in treatment protocols.
Future research aims to refine HIPEC techniques, identify biomarkers for patient selection, and explore novel therapeutic combinations.
Conclusion
Epithelial ovarian cancer, with its propensity for peritoneal spread, poses a formidable clinical challenge. However, the integration of cytoreductive surgery and HIPEC into standard care has revolutionized outcomes, offering improved survival and quality of life for patients. As evidence continues to mount, HIPEC represents a beacon of hope in the battle against this devastating disease.
Tags
- Ovarian Cancer
- Peritoneal Carcinomatosis
- HIPEC
- Cytoreductive Surgery
- Advanced Cancer Treatment
- Oncology Innovations
- Intraperitoneal Chemotherapy
- ESMO Guidelines
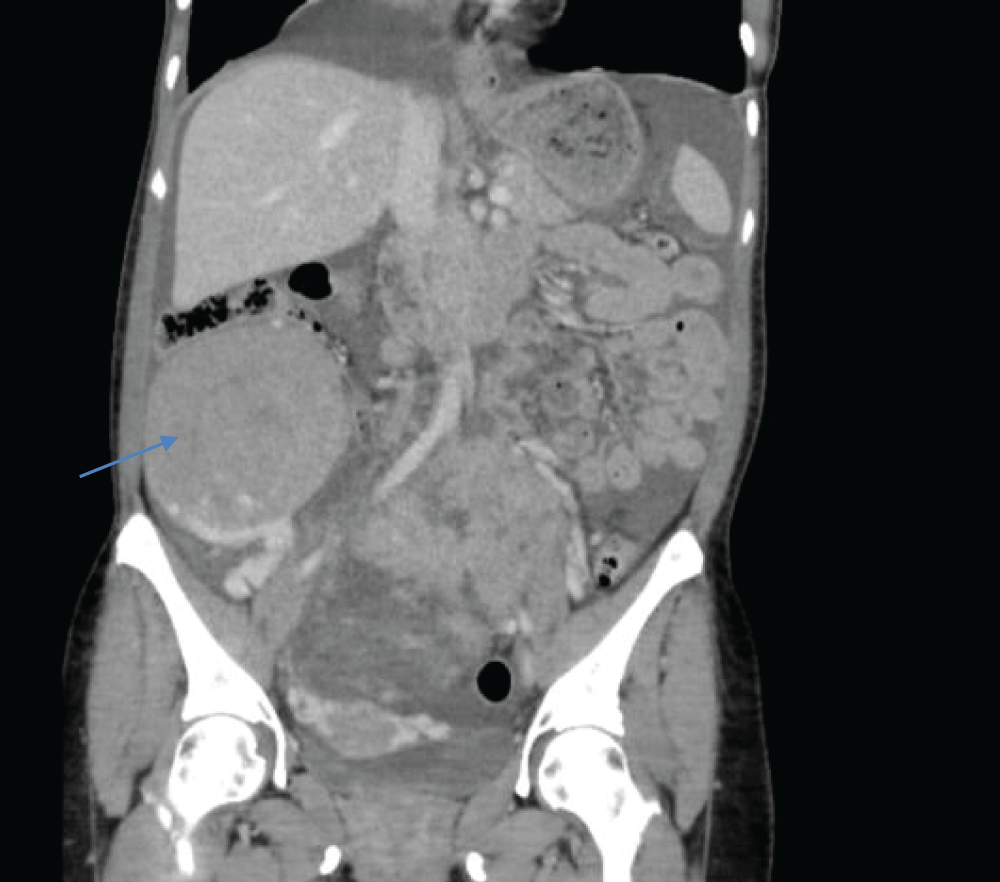
Figure 1: The tumor (→) contacts and displaces intestinal loops superiorly, as well as large retroperitoneal vessels.
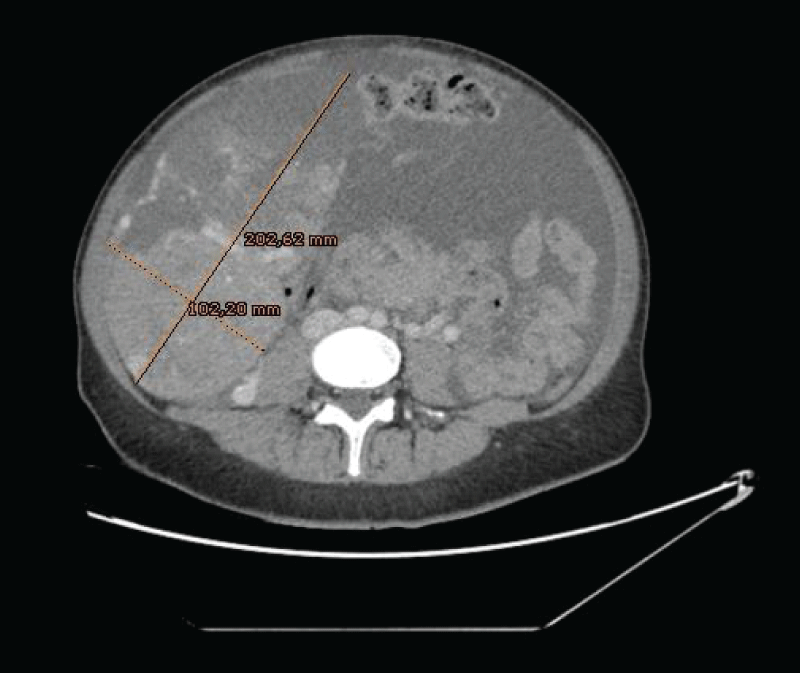
Figure 2: Large, vascularized, and heterogeneous masses that depended on both ovaries, the one on the right side measured 20 x 10 cm.
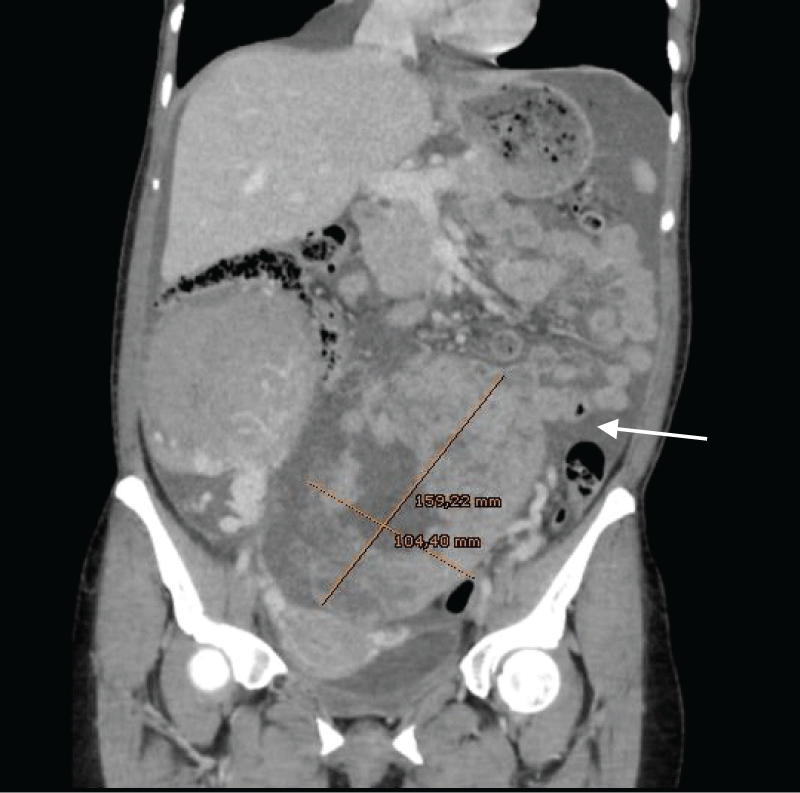
Figure 3: Ascitic fluid suggestive of peritoneal carcinomatosis (→). Large, vascularized, and heterogeneous masses that depended on both ovaries, the one on the left side measured up to 16 x 10 cm.
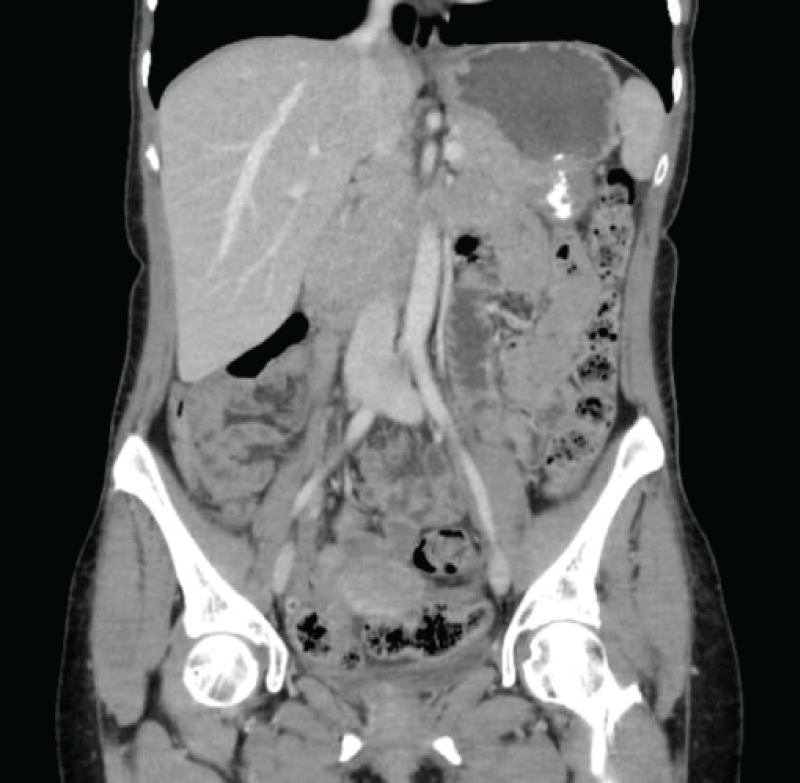
Figure 4: Postsurgical changes in the pelvic area concerning bilateral oophorectomy. Complete disappearance of previously existing ascites.
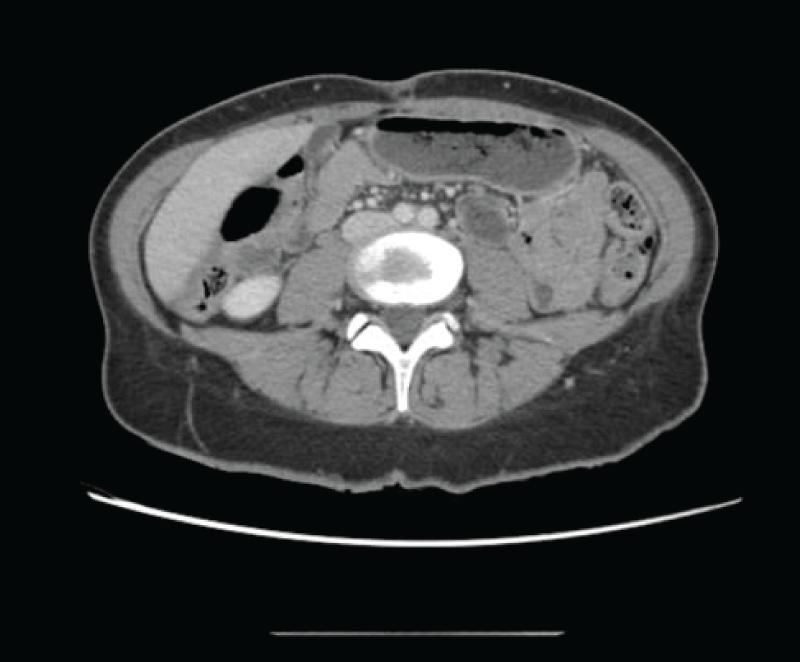
Figure 5: Subtly granular appearance of the peritoneal fat, which does not allow to conclusively rule out metastatic carcinomatous dissemination.
