Screening for Sexually Transmitted Infections in Adolescents with Genitourinary Complaints: Is There a Still Role for Endocervical Gram Stains?
Introduction Adolescents are disproportionately affected by sexually transmitted infections (STIs), with significant implications for their reproductive and overall health. Among the STIs commonly diagnosed are Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis. With nearly 20 million new STI cases annually in the United States, adolescents aged 15-24 represent a substantial portion of this burden. This blog explores the relevance of traditional diagnostic tools like endocervical Gram stains and the challenges faced in emergency departments (EDs) when addressing these critical public health concerns.
Adolescents and the Burden of STIs
Adolescents face unique barriers in accessing healthcare for STI prevention, diagnosis, and treatment. Confidentiality, stigma, and costs often hinder proactive health management. STIs like chlamydia and gonorrhea, if untreated, can lead to complications such as pelvic inflammatory disease (PID), ectopic pregnancies, and infertility.
Emergency departments often serve as the first point of contact for adolescents presenting with symptoms such as abdominal pain, unusual discharge, or genitourinary complaints. However, the ED environment poses challenges, including delayed test results and potential overtreatment or undertreatment due to empirical decision-making.
Endocervical Gram Stains: An Outdated Diagnostic Tool?
Endocervical Gram stains were once a cornerstone of STI diagnostics, offering rapid identification of bacterial pathogens. However, their sensitivity and specificity have been questioned. In a recent study involving over 1,300 adolescent females, the sensitivity of Gram stains for detecting chlamydia, gonorrhea, and trichomoniasis ranged from a mere 5.7% to 35.9%. While the test provides immediate results, its low diagnostic accuracy raises concerns about its continued use in clinical settings.
Key Study Findings:
- Population: Adolescents aged 13-19 presenting with genitourinary complaints.
- Methods: Diagnostic performance of Gram stains compared to Polymerase Chain Reaction (PCR) assays.
- Results: Sensitivity and specificity of Gram stains were 28.7% and 78.1%, respectively.
- Implications: High rates of overtreatment and undertreatment highlight the need for more reliable diagnostic methods.
The Role of Emergency Medicine
Emergency physicians often rely on clinical judgment due to the unavailability of rapid, accurate test results. This reliance can lead to:
- Overtreatment: Empirical use of antibiotics increases the risk of antibiotic resistance.
- Undertreatment: Missed diagnoses contribute to continued STI transmission and complications.
Improving diagnostic accuracy in the ED requires integrating point-of-care testing, like rapid DNA probes, with established guidelines.
Gynecology and Pediatrics Collaboration
Gynecology and Pediatrics play pivotal roles in STI prevention and management. Routine screenings, especially for sexually active adolescents, can mitigate the long-term impact of untreated infections. Pediatricians, often the first healthcare providers for adolescents, must advocate for preventive education and regular testing.
Modern Diagnostic Advances
Polymerase Chain Reaction (PCR) assays have emerged as the gold standard for STI detection, boasting high sensitivity and specificity. Despite their efficacy, PCR tests face logistical challenges, such as higher costs and longer turnaround times compared to traditional methods. Point-of-care tests, capable of delivering accurate results within hours, represent a promising alternative.
Case Study: Success with Point-of-Care Testing A pilot program integrating rapid STI testing in pediatric emergency departments reported:
- Reduced overtreatment rates by 30%.
- Improved patient follow-up compliance.
- Shortened time to diagnosis and treatment.
Addressing the Public Health Challenge
Key Recommendations:
- Education and Awareness: Schools and community programs should emphasize STI prevention and the importance of early detection.
- Accessible Testing: Mobile clinics and telehealth consultations can bridge gaps in healthcare access for underserved populations.
- Policy Reforms: Implementing standardized protocols for STI screening in EDs can ensure consistent care.
Integrating Research into Practice
Studies, such as the one conducted at Michigan State University and Corewell Health, underscore the critical need to reassess traditional diagnostic tools. Emergency departments and clinics must adopt evidence-based practices to improve outcomes for adolescent patients.
Conclusion
The burden of STIs among adolescents necessitates a collaborative approach spanning Gynecology, Pediatrics, and Emergency Medicine. While endocervical Gram stains have historical significance, their limitations call for the adoption of modern diagnostic technologies. Addressing these gaps will require systemic changes in how adolescent sexual health is managed, ensuring timely and accurate diagnosis to prevent complications and transmission.
References
For detailed study data and additional insights, explore:
- Full Text Article
- PDF Version
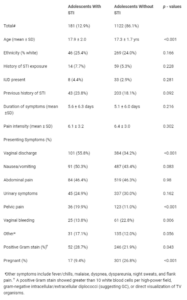 Table 1: Demographics and presenting complaints in adolescent women with and those without documented sexually transmitted infection (STI).
Table 1: Demographics and presenting complaints in adolescent women with and those without documented sexually transmitted infection (STI).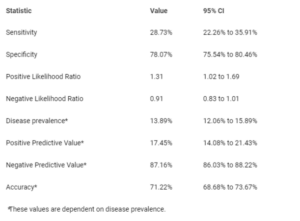 Table 2: Diagnostic indices for endocervical Gram smears in the diagnosis of STIs in a female adolescent population with genitourinary complaints.
Table 2: Diagnostic indices for endocervical Gram smears in the diagnosis of STIs in a female adolescent population with genitourinary complaints.
