Prevalence of Non-specific Low Back Pain Among Chinese Healthcare Workers (Surgeons and Surgical Nurses): A Multi-Center Survey Study
Introduction
Low Back Pain (LBP) remains a significant global health issue, affecting millions of individuals across various age groups. In the healthcare sector, this condition is particularly prevalent among surgeons and surgical nurses due to the physical demands of their roles. A recent study titled “Prevalence of Non-Specific Low Back Pain Among Chinese Healthcare Workers (Surgeons and Surgical Nurses): A Multi-Center Survey Study” sheds light on the factors contributing to LBP in healthcare professionals and suggests practical solutions to mitigate this occupational hazard.
Explore the full study: PDF | DOI
Understanding Non-Specific Low Back Pain in Healthcare Workers
Non-specific LBP is characterized by pain that is not linked to a specific anatomical cause. In healthcare workers, this condition can arise from prolonged standing, repetitive movements, and improper posture during surgical procedures. The study conducted across six hospitals in China provides comprehensive insights into the prevalence and risk factors associated with LBP in surgeons and surgical nurses.
Key Findings of the Study
The study involved a total of 250 participants, including both surgeons and surgical nurses, with the following key findings:
- Mean Age: 45.8 years
- Gender Distribution: 81.2% male and 18.8% female
- Average Body Mass Index (BMI): 25.07 kg/m²
- Working Hours: Participants reported working between 50 to 55 hours per week
- Prevalence of Mild LBP: 90.4% of participants experienced mild LBP
The study highlighted that orthopedic surgeons were at the highest risk of developing LBP, primarily due to long working hours and incorrect posture during procedures.
Risk Factors Associated with LBP in Healthcare Professionals
The study identified several risk factors contributing to LBP among healthcare workers:
- Long Working Hours: Healthcare professionals often work extended shifts, which can increase the risk of LBP.
- Improper Posture: Incorrect body posture during surgeries and other medical procedures is a significant risk factor.
- Body Mass Index (BMI): Higher BMI was associated with an increased risk of LBP.
- Lack of Physical Activity: Healthcare workers who did not engage in regular physical exercise were more likely to experience LBP.
 Figure 1: STROBE diagram of participants with LBP.
Figure 1: STROBE diagram of participants with LBP.
The diagram above illustrates the participant selection process, including inclusion and exclusion criteria.
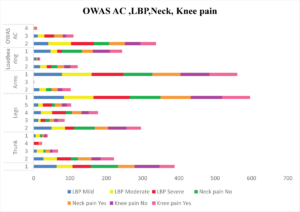 Figure 2: Working posture in HCP with the level of LBP, neck pain, and knee pain based on OWAS AC subgroups.
Figure 2: Working posture in HCP with the level of LBP, neck pain, and knee pain based on OWAS AC subgroups.
Assessment Tools Used in the Study
The researchers used several tools to assess the severity of LBP and the associated risk factors:
- Visual Analog Scale (VAS): A tool used to measure pain intensity.
- Quebec Back Pain Disability Scale (QBPDS): Used to assess the impact of LBP on daily activities.
- Ovako Working Posture Assessment System (OWAS): Evaluates the working posture of healthcare professionals.
The results showed that improper posture, particularly trunk and leg positions, significantly contributed to the severity of LBP.
Impact of LBP on Healthcare Workers
LBP affects not only the physical well-being of healthcare workers but also their professional performance. The study revealed that:
- Neck Pain: 46% of participants reported experiencing neck pain alongside LBP.
- Knee Pain: 26% of participants experienced knee pain.
- Reduced Productivity: LBP can lead to reduced efficiency and increased absenteeism in the workplace.
To address these issues, healthcare institutions must implement preventive measures to reduce the prevalence of LBP.
Preventive Measures to Address LBP
The study suggests several strategies to prevent and manage LBP in healthcare professionals:
- Ergonomic Adjustments: Ensuring that workstations and surgical equipment are ergonomically designed to minimize strain.
- Regular Physical Exercise: Encouraging healthcare workers to engage in physical activities that strengthen the back muscles.
- Education and Training: Providing training on proper posture and body mechanics during medical procedures.
- Workplace Policies: Implementing policies that promote regular breaks and reduce prolonged standing during shifts.
Table: Demographic and Anthropometric Characteristics of the Study Sample
Characteristic | Mean | Standard Deviation | Median | Range |
Age | 45.8 | 11.0 | 45.0 | 43.0 |
BMI | 25.07 | 1.49 | 24.98 | 8.24 |
The Role of Health Policies in Addressing LBP
Health policies play a crucial role in addressing occupational hazards like LBP. By implementing targeted policies, healthcare institutions can create a safer working environment for their staff.
Policy Recommendations:
- Mandatory Ergonomic Training: All healthcare workers should receive mandatory training on ergonomics.
- Regular Health Assessments: Conduct periodic health assessments to identify early signs of LBP.
- Flexible Work Schedules: Implement flexible work schedules to reduce prolonged working hours.
 Figure 3: Percentages of OWAS AC based on designations.
Figure 3: Percentages of OWAS AC based on designations.
The figure shows the distribution of OWAS action categories among different healthcare professionals.
Conclusion
The prevalence of LBP among healthcare workers highlights the need for immediate action to address this occupational hazard. By understanding the risk factors and implementing preventive measures, healthcare institutions can improve the well-being and productivity of their staff.
Explore the full study for more detailed insights: PDF | DOI
This blog post aims to raise awareness about the prevalence of LBP in healthcare settings and encourage healthcare institutions to take proactive steps to address this issue.
